My name is Nikki Mather. I am a Board Certified Lactation Consultant (IBCLC) who specialises in support families with all feeding methods, and help navigate the challenges which families face every day with feeding their babies. I offer support on Zoom and in person in the North West of England primarily in Cheshire, Greater Manchester and Merseyside.
Have you been told your breastfeeding latch great (or bottle if that’s your chosen method) yet you still have challenges with reflux, colic, wind, CMPA, allergies?
This is a little different to my usual blog musings. It’s a little close to heart for many of us working in the infant feeding realms you see, and we witness these things happen in our day to day work.
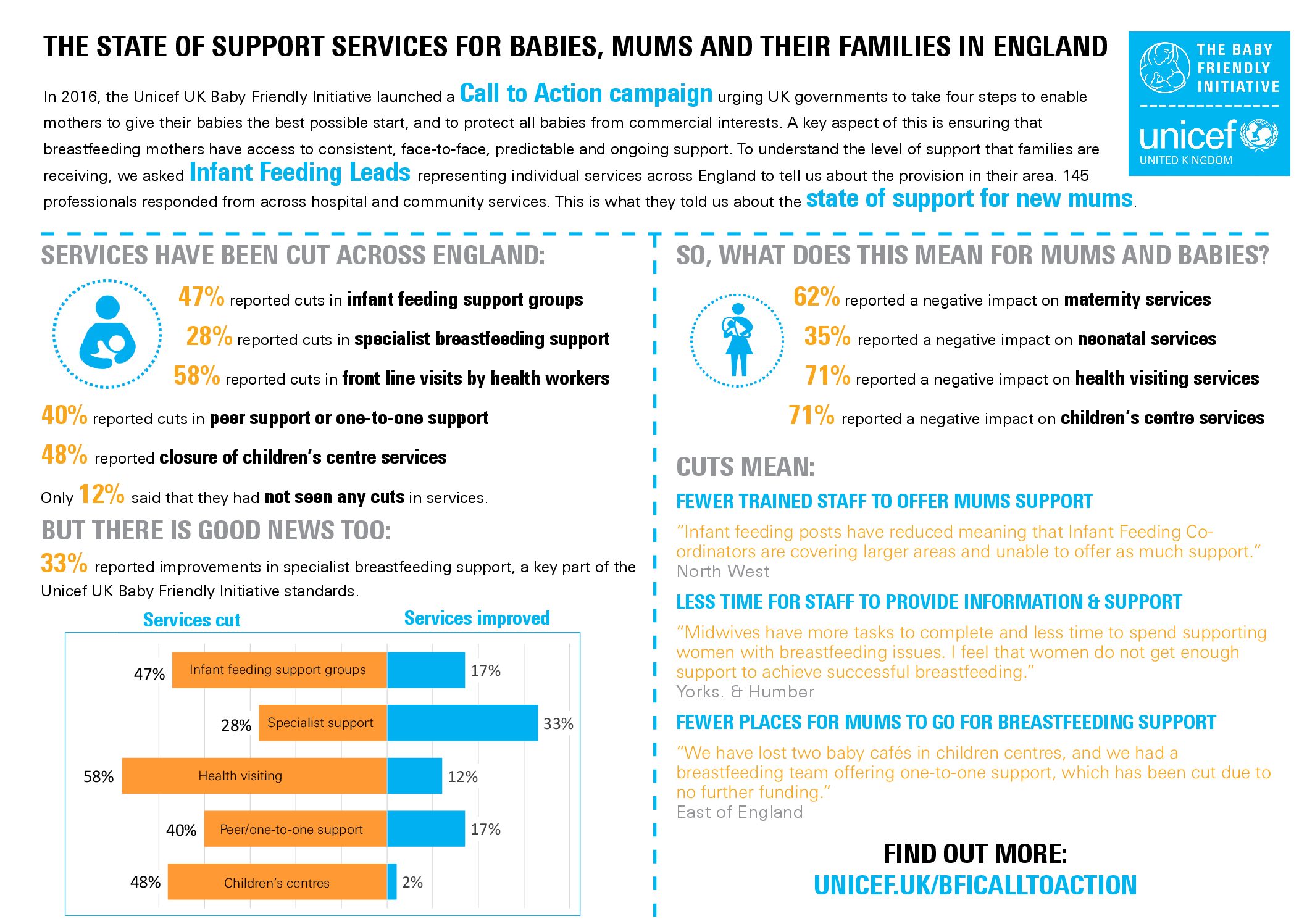
Infant feeding is such an important part of our parenting journey and due to the cuts and lack of funding in infant feeding, this leaves so few people trained in basic breastfeeding support, let alone the complex stuff which comes up, parents are often left wondering what they might be able to do to improve their situation without the support to do so. If you think breastfeeding support is lacking, bottle feeding support is non-existent. Support for people wishing to feeding their babies as non-gestational parents even less support as training is lacking so much in the world of infant feeding as a whole, everyone can be left in the dark and not knowing where to turn for support when babies need feeding.
We find Facebook groups are full of peer support in the form of mum to mum and parenting groups offering words of encouragement, support and chat 24 hours a day which is great for moral support and a virtual hug at 3am when things are just exhausting.
Somebody else is also on the twilight shift, trying to crack that perfect latch. We also witness within those groups parents and babies who need individualised support, which is face to face and from a specialist. One example, quite frankly a scary one, is to see parents of extremely underweight babies told to “just breastfeed, hun”, with no concern or request for review from a healthcare professional, breastfeeding counsellor or IBCLC. Latching onto the bottle is also tricky for some babies with reflux, colic, CPMA and allergies being overdiagnosed by the second.
What often happens far too frequently (just reading Facebook groups is enough to gather evidence on this) is that across the UK, no real assessment occurs, any of the parents concerns are not listened to and are often dismissed or trivialised, and you just have to continue because your baby’s latch is fine…
More and more frequently we hear of peer supporters, Breastfeeding Counsellors, IBCLCs, midwives, health visitors and even dentists telling parents to ” just feed feed feed”. This information is all fine and well for a term baby who is drinking well at the breast and having frequent wet and dirty nappies and gaining weight. Feed the baby is always the first rule, but fed is not best as Dr Amy Brown discusses here.
On the other end of the spectrum, blanket infant feeding information is not so ok when the opposite is happening and the signs parents are reporting show a baby who isn’t transferring milk as well as they could. What are parents to do? Where do they turn when they’ve already consulted *insert infant feeding person or Professional* and been told all is well when the actual evidence says differently? Assessment of medical history, observing an entire feed, taking a history of pregnancy, birth and what has happened up to now and analysing all of this cannot be done in a 15 minute session.
Is baby drinking well and regularly – 8-12 times a day?
Are you and baby comfortable and attaching well at the breast, chest or bottle in a position which works for you?
Has anybody observed a full feed to check this and reassure you and explain how to recognise the signs your baby is transferring milk well? How many wet and dirty nappies? Are you and your baby getting sleep between feeds? Are their hands relaxed and open, and does your baby sleep after a feed?
Is baby coughing, spluttering during feeds or refusing to feed?
Has reflux, CMPA, allergies been diagnosed or has your baby been prescribed medication or specialist formula?
As a general rule of thumb, a newborn baby in the first 6-8 weeks of life who is hydrated and feeding well will:
- have 6-8 wet nappies per day,
- a minimum of 2 dirty nappies per day (3/4 or more is also normal) of good consistency and colour,
- show signs of relaxation (hands unclasped and floppy) towards the end of a feed,
- sleep well between feeds or remain peaceful and are calm if they remain awake for a time afterwards.
Feeding plans written by Lactation Consultants are sometimes put in place where babies have a tricky start because of their birth situations, a delay in milk coming in or anatomical issues like tongue tie or cleft palate. Babies may be gaining too little or too much weight. Where a large weight loss in the early days occurs, those short term combination feeding plans are valuable in protecting milk supply and reduce the risk of deydration and the problems that could occur. Pumping and breastfeeding, an element of topping up with expressed breastmilk or artifical infant milk can support the dyad when early signs of problems haven’t been recognised
Sometimes babies will be finger feeding and breastfeeding or bottle feeding, syringe feeding or using an SNS. A combination of all of these methods is sometimes used – which can be utterly confusing for somebody who isn’t trained in using supplemental support and may dismiss their validity. Triple feeding is one of the most difficult plans to set but is sometimes a short term necessity.
Which qualifications are held by the people providing you with infant feeding support? There are several examples in other blogs about the difference between a peer supporter, a Breastfeeding Counsellor and a IBCLC. And even between all of those roles, there are vast differences across the country in the training and experience each individual may have.
It is important to note that whilst some areas have specialist trained midwives and h
ealth visitors, many areas do not and parents with infant feeding problems should be referred to somebody who can assess infant feeding where a problem arises because it is not all about the latch. I recently met a “Infant Feeding Specialist Health Visitor” who openly admitted she had only ever done the BFI 3 day training at her local hospital several years ago (this is now a 5 day course)
As a new parent, you and your baby are learning, you are getting to know each other and how these things work for you personally. Knowing where to find the correct support for individual situations, tailored to you, as well as the basic information about infant feeding is important to your journey.
Funds are cut continually and services are overstretched in maternity and community health visiting. This often results in nobody being qualified, no specialist training in infant feeding or assessment (remembering experience and training are not equal across the country). Throughout the training I have attended myself over the years, it is often relayed to us that should we see something that is beyond our remit, referral pathways to somebody else who can provide additional help should be the next step. If you do not know the answer, if you need more help, if you aren’t trained, say so, and appropriately refer to somebody who is.
In an ideal world that’s how it should work…..instead a quick peek is had and parents are often told “you’re baby’s latch is GREAT!” because the subtle differences between a baby hanging out at the breast receiving very little and a baby feeding effectively are missed by the untrained or inexperienced eye. Parents then believe they’re doing all they can and when things don’t go to plan they have no explanation because somebody told them things were perfect.
Below you will find highlighted some of things we see and hear in our work with parents and babies in lactation support.
Your baby’s latch is great…..
- Your nipples look like a brand new Heather Shimmer and feel as though they may fall off if you ever feed your baby again, yet your baby’s latch is great.
- Your baby is coughing, spluttering and refusing to drink from bottle
- Your latch is great when you feel like a cheese grater is attached to your breast and you are convinced a vice would be less painful.
- Bleeding, agonising, lacerated nipples – your latch is great!!!
- Your baby’s latch is great if they stop feeding due to ‘fast letdown’
- Your baby’s red book shows slow or static weight gain, and baby’s latch is great.
- Your shoulders ache as your baby feeds for an hour and comes back to nurse again after a 15 minute break, the latch is great!
- Your baby hasn’t slept in the first 72 hours hours of life for more than 5 minutes at once, your baby’s latch is great.
- Your baby has slept soundly for 8 hours and fed 4 times today, your latch is great.
- You’ve seen no dirty nappies for 3 days, your latch is great.
- Wet nappies are few, but your latch is great.
- Five minute feeds and hour long naps before hunger strikes again, your latch is great.
- You’ve only eaten once today and had no rest between feeds, you’re doing great and so is your latch!
- After a big, wide attachment which you’ve nailed with military precision, your baby slips to the end of your nipple, and so your latch is great.
- No swallowing and lots of sucks, your baby’s latch is great.
- Nipple in babies mouth? Your latch is great!
From Alice: your breast is so swollen-full of milk that your nipple won’t fit in your babies mouth, but your latch is great.
You might recognise some of these scenarios or feel you’d like to add to this list, contact me if you’d like to add your own.
Finding the support you need can be difficult and sometimes confusing for new parents who are not sure who is and is not qualified to provide basic support or when things might need more specialist help. Some areas are a postcode lottery with infant services being cut and training stopped. There are some great places to find support across the UK from online resources, national breastfeeding helplines and asking parents for reviews of those services local to you. Effective feeding signs are the key to success, not what your breastfeeding latch looks like to somebody else.